When the brain’s fragile balance is disrupted by an ill wound, a neurostorm (alternatively referred to as paroxysmal sympathetic hyperactivity or autonomic dysfunction syndrome) can strike — and it’s awful: bursts of rapid heartbeat, fever, perspiration, shaking and other savage, unstoppable reactions.
Imagine this friend who is banging their head and then suddenly seems to be experiencing a panic attack that will not abate — that’s what doctors worry about.
It hits thousands every year and needs immediate attention because figuring out the causes, knowing the signs, and starting treatment early can bring a person back on their feet versus continued harm.
What Is a Neurostorm?
A neurostorm is your body’s “fight or flight” switch stuck on overdrive after a traumatic brain injury or stroke.
Your heart races suddenly, blood pressure shoots up, breathing accelerates, muscles tense, and body temperature ascends—all at once.
It’s as if the body gas pedals without brakes.
Normally, your brain keeps things balanced between “go mode” (the sympathetic system) and “chill mode” (the parasympathetic system), but when that balance breaks, chaos takes over.
Doctors first noticed this back in the 1950s, and today we know it can hit up to a third of patients with severe brain injuries.
It’s one of the scariest challenges ICU teams face—and spotting it fast can save lives.
The Science Behind Neurostorms
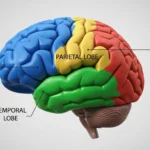
Researchers continue to try to figure out exactly how and why neurostorms occur, but this is the short version: when brain areas that control automatic activities—such as the hypothalamus and brainstem—are impaired, the “calm down” signals fail to reach them.
Think of cutting the brakes on a runaway vehicle—that’s what occurs to the stress system in the body.
Even small things, such as rolling someone over in bed or bathing him or her, can lead to a titanic overreaction: racing heart, sweating, trembling, the whole shebang.
Brain scans show that many patients with neurostorms have something called diffuse axonal injury—tiny tears in the brain’s wiring that mess up how different regions talk to each other.
With the communication lines down, the body’s “go” system runs wild, creating the storms doctors struggle to control.
Recognizing the Signs and Symptoms
Spotting a neurostorm fast can make a huge difference — it’s like catching a sudden thunderstorm before it floods everything.
Here’s what doctors watch for, explained like I’d tell a curious teen:
Cardiovascular Symptoms
These are the theatrics ones: the heart just takes off — imagine running-from-a-dog speed — usually above 120 beats per minute.
Blood pressure shoots to terrifying highs, and the individual sweats even in a chilly room.
It’s as if your body is revving up an engine that will not shut off.
Respiratory Changes
Breathing can turn shallow and fast — more than 30 breaths a minute — even when oxygen levels aren’t the problem.
Picture someone hyperventilating from panic, but it’s happening without that emotional trigger.
Temperature Dysregulation
Fever can suddenly arise from nowhere at all, sometimes over 101°F (38.3°C) in size, with no infection lurking in the background.
It’s like the body’s thermostat broke down.
Muscular Symptoms
This can be flat-out frightening: arms and legs can stiffen into abnormal positions (severe posturing), muscles become immobilized, and acutely painful involuntary spasms (dystonia) can happen.
Picture a puppet whose strings are being pulled taut — except on your friend’s muscles.
Pupillary Changes
Eyes can give clues too — pupils may dilate and respond poorly to light, which is another sign the autonomic system is misbehaving.
Risk Factors and Vulnerable Populations
Not everyone who gets a bad brain injury will have a neurostorm — but some people are way more likely to.
Think of it like lightning: it can strike anywhere, but some conditions make the perfect storm. Here’s what doctors look out for:
Traumatic Brain Injury Severity
This is the biggest red flag.
When someone comes into the hospital with a Glasgow Coma Scale (GCS) score of 8 or lower — meaning they’re barely conscious — the chances of a neurostorm shoot up.
The GCS is basically a quick “how awake are you?” test, and the lower the score, the rougher the road ahead.
Age Demographics
Weirdly enough, neurostorms tend to hit younger people harder — usually those between 15 and 35.
Doctors think it’s because younger bodies have stronger “fight-or-flight” systems. In other words, your nervous system is too good at freaking out.
Injury Mechanisms
It’s more a matter of how the brain was hurt rather than what it experienced.
Diffuse axonal injury — small tears in the brain’s wiring system — is a prime offender.
Such injuries usually occur in car accidents or large falls. It’s as if the brain’s quiet-down wires are frictioned the wrong way, and suddenly the “calm down” messages can’t get through.
Location of Brain Damage
If the injury is to areas such as the brainstem, hypothalamus, or basal ganglia (the regions that regulate your body’s automatic functions), the risk increases huge time.
It’s like blowing up the headquarters that makes your body function right.
Timing of Symptoms
Neurostorms tend to occur within the first two weeks after injury — typically days 4 to 7.
That is when physicians are on high alert. When the symptoms begin to degenerate on those days, there is a good possibility a storm is raging.
Diagnostic Approaches and Assessment Tools
Diagnosing a neurostorm is more like detective work than a single lab test — doctors first rule out other “copycat” causes (infections, blood clots, drug withdrawal) before saying it’s PSH.
The PSH-Assessment Measure (PSH-AM) is the default checklist: it scales six major signs — heart rate, breathing, blood pressure, temperature, sweating, and posturing — and then applies a likelihood tool that inquires for timing, episode duration, and other causes elimination.
Consider the Clinical Features Scale to be the crime scene photos and the Diagnosis Likelihood Tool to be the lineup of suspects.
Continuous monitoring — heart, temp, and motor checks around the clock — gives the team the pattern they need to predict storms and test if treatments are actually calming things down.
In short: rule out impostors, score the signs, watch closely, and treat the pattern.
Treatment Strategies and Management
Managing a neurostorm is like knocking down a wildfire from several angles at once — you need fast medicine, smart surroundings, gentle movement, and constant watching.
Pharmacological Interventions
Medications are the first line of defense: beta-blockers (propranolol) slow down the heart and blood pressure, opioids and benzodiazepines soothe the overexcited nervous system and muscles, and medications such as gabapentin or bromocriptine even prevent storms from happening as often.
Consider them like all the various gadgets in a fireman’s bag — each performs some vital function.
Environmental Modifications
A calm, dim, low-noise room and minimal handling can stop tiny triggers from turning into full storms.
I once watched a nurse cut a patient’s episode in half just by slowing down and turning the lights off for a few minutes — tiny changes matter.
Physical Interventions
Careful positioning, gradual movement through the range of motion, and gradual mobilization avoids painful positions and maintains working joints without irritating symptoms — such as stretching rather than yanking.
Monitoring and Adjustment
Staff monitors vitals closely and adjusts meds accordingly as needed according to what appears to work, monitoring for side effects.
That is to say: drug to quiet the storm, setting to avoid sparks, motion to protect the body, and ongoing observation to remain one step ahead.
Long-Term Outcomes and Recovery
Neurostorms can really shake up the road to recovery after a brain injury.
Patients who go through them usually stay in the hospital longer and need more rehab — it’s like the brain has to fight two battles at once: healing from the injury and calming its overactive systems.
But here’s the hopeful part: with quick action and good care, many people slowly get better over weeks or months.
As the brain heals, it often relearns how to keep the body’s “fight-or-flight” system under control.
Some patients make a full comeback, while others may still have milder flare-ups that need long-term management.
The best recoveries usually happen when the storm is caught early, the brain injury isn’t too severe, and the patient is younger — their brains are just more flexible and faster to adapt.
On the flip side, if the condition is missed or the damage runs deep, recovery can be tougher and take much longer.
But even then, every small step forward is a victory worth celebrating.
Conclusion
Neurostorms are a scary but treatable complication after serious brain injury — the body’s “fight-or-flight” goes haywire, but quick recognition and a smart team can calm it.
Think of it like a storm you can learn to weather: doctors use meds, quiet rooms, and close monitoring to stop the chaos, and many people gradually get better.
I’ve seen nurses and doctors steady a patient just by slowing everything down — small actions matter.
If you’re caring for someone with a brain injury, speak up the moment you notice clustered signs (fast heart, fever, rigid muscles); early action really changes the outcome.