Adrenal cortex cancer—called adrenocortical carcinoma (ACC)—is super rare but seriously tough.
Only one or two people in a million get it each year, but when it shows up, it doesn’t mess around. Knowing the signs and basics really matters, because catching it early can make a big difference.
Think of this as a quick, no-nonsense guide from someone who’s seen how powerful knowledge can be.
What Is Adrenal Cortex Cancer?
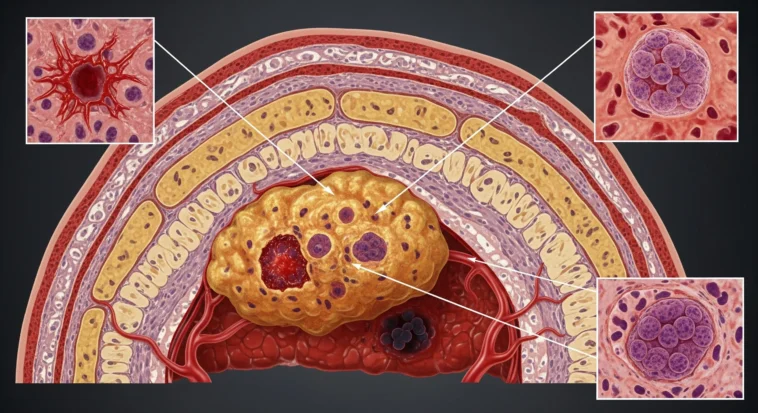
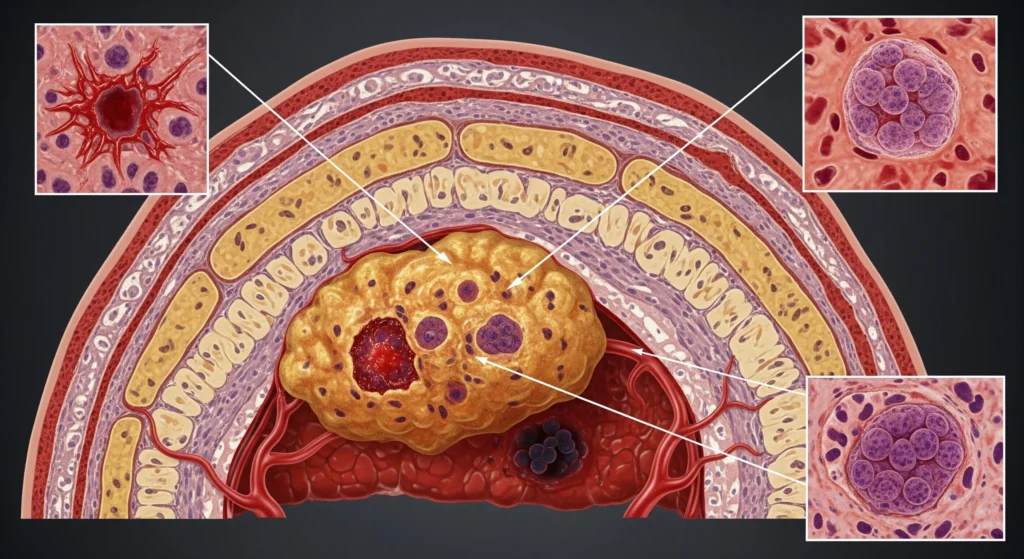
Picture two tiny, triangle-shaped glands sitting on top of your kidneys.
Those are your adrenal glands, and they’re like the body’s behind-the-scenes managers—handling stress, energy, blood pressure, and even puberty hormones.
The adrenal cortex is the outer layer, and it makes hormones like cortisol and adrenaline helpers. In adrenocortical carcinoma, cells in that layer go rogue and grow out of control.
Unlike common, harmless adrenal lumps (which many adults have and never notice), ACC is rare and dangerous.
Some ACC tumors are “functional”, meaning they pump out way too many hormones—causing wild symptoms. Others are “non-functional” and stay quiet until they grow big or spread. Either way, this cancer is aggressive, which is why doctors take it very seriously.
Recognizing the Signs and Symptoms
Here’s the tricky part about adrenal cortex cancer: it’s a master of disguise. Early on, it can feel like “meh, something’s off,” which is why people sometimes ignore it.
Hormone-Related Symptoms
Some tumors act like broken hormone factories and flood the body with signals it never asked for:
- Cushing’s syndrome: Too much cortisol. Think sudden weight gain in the face and belly, purple stretch marks (not the gym kind), bruising easily, weak muscles, high blood pressure, and mood swings that make you feel like a totally different person.
- Conn’s syndrome: Too much aldosterone. Blood pressure that won’t chill, low potassium, muscle weakness, peeing a lot, and being constantly thirsty.
- Virilization: Extra male hormones. In women, this can mean facial hair, a deeper voice, hair loss, or messed-up periods. In kids, it can look like puberty hitting the fast-forward button.
- Feminization: Rare, but real. Extra estrogen can cause breast growth in men, low sex drive, and erectile problems.
Non-Hormonal Symptoms
If the tumor isn’t messing with hormones—or just gets big—it can cause:
- Ongoing belly or back pain
- A noticeable lump in the abdomen
- Feeling full all the time
- Unexplained weight loss
- No appetite
- Random fevers
If your body is sending loud, confusing signals—especially hormone changes plus belly pain—don’t ignore it. Getting checked early can be a game-changer.
Understanding Risk Factors and Causes
While the exact cause of adrenal cortex cancer remains unknown, researchers have identified several risk factors that may increase the likelihood of developing this disease.
Genetic Syndromes
Certain inherited genetic conditions significantly increase the risk of ACC:
- Li-Fraumeni syndrome: A hereditary disorder caused by mutations in the TP53 gene, substantially increasing cancer risk, including adrenocortical carcinoma.
- Beckwith-Wiedemann syndrome: A genetic disorder characterized by overgrowth, which increases the risk of various childhood cancers including ACC.
- Multiple endocrine neoplasia type 1 (MEN1): An inherited condition causing tumors in multiple endocrine glands.
- Familial adenomatous polyposis (FAP): Primarily associated with colon cancer but also linked to increased adrenal cancer risk.
Other Risk Factors
- Age: ACC has a bimodal distribution, with peaks occurring in children under five years old and adults in their 40s and 50s.
- Gender: Women are slightly more likely to develop functional adrenocortical carcinomas than men.
- Tobacco use: Some studies suggest smoking may increase risk, though the connection is not definitively established.
It’s important to note that having one or more risk factors doesn’t guarantee you’ll develop adrenal cortex cancer, and many people diagnosed with ACC have no identifiable risk factors.
Diagnostic Process: How Adrenal Cortex Cancer Is Detected
Diagnosing adrenal cortex cancer involves a comprehensive approach combining clinical evaluation, laboratory tests, and imaging studies.
Physical Examination and Medical History
Your healthcare provider will conduct a thorough physical examination and review your medical history, paying particular attention to symptoms suggesting hormonal imbalances or abdominal masses.
Laboratory Tests
Blood and urine tests measure hormone levels to determine if the tumor is functional:
- 24-hour urine collection to measure cortisol and other hormone metabolites
- Blood tests for cortisol, aldosterone, DHEA-S, testosterone, and estrogen
- Electrolyte panels to check for potassium abnormalities
- Blood glucose and lipid profiles
Imaging Studies
Various imaging techniques help visualize the tumor and determine if cancer has spread:
- CT (Computed Tomography) scans: Provide detailed cross-sectional images of the adrenal glands and surrounding structures, helping determine tumor size and characteristics.
- MRI (Magnetic Resonance Imaging): Offers excellent soft tissue contrast and can help distinguish between benign and malignant tumors.
- PET (Positron Emission Tomography) scans: Particularly useful for detecting metastatic disease and assessing treatment response.
- Adrenal vein sampling: A specialized procedure sometimes used to determine which adrenal gland is producing excess hormones.
Biopsy Considerations
Unlike many other cancers, biopsy is rarely performed for suspected adrenal cortex cancer because of the risk of spreading cancer cells. Diagnosis is typically made through imaging characteristics and hormone studies, with definitive diagnosis confirmed after surgical removal.
Staging and Prognosis
Adrenal cortex cancer is staged using the TNM (Tumor, Node, Metastasis) system, which helps determine treatment approaches and predict outcomes.
Stage I: Tumor is 5 centimeters or smaller and confined to the adrenal gland.
Stage II: Tumor is larger than 5 centimeters but still confined to the adrenal gland.
Stage III: The tumor has grown into nearby tissues or spread to nearby lymph nodes.
Stage IV: Cancer has spread to distant organs (most commonly the liver, lungs, or bones) or to distant lymph nodes.
Prognosis varies significantly based on stage at diagnosis. Early-stage disease (I and II) has a more favorable outlook, with five-year survival rates ranging from 60-80% for stage I disease.
Unfortunately, many patients are diagnosed with advanced-stage disease, where five-year survival rates drop to 10-35% for stage III and less than 10% for stage IV.
Factors affecting prognosis include:
- Stage at diagnosis
- Completeness of surgical removal
- Tumor size and growth rate
- Hormone production status
- Age and overall health
- Response to treatment
Treatment Options: A Multidisciplinary Approach
Treating adrenal cortex cancer is like assembling an Avengers team—no single hero can do it alone.
Doctors from different specialties work together to attack the cancer from every angle, and that teamwork really matters.
Surgery
Surgery is the main event. If the cancer hasn’t spread, removing the adrenal gland (called an adrenalectomy) gives the best shot at a cure. Surgeons aim to take everything—no cancer left behind. Sometimes that means removing nearby tissue too. It’s intense, but it saves lives.
Medication Therapy
- Mitotane: This drug is kind of a specialist—it’s made just for adrenal cancer. It hunts down adrenal cells, including leftover cancer cells.
- Chemotherapy: For cancer that’s spread, chemo teams up with mitotane to slow things down and fight back.
- Targeted therapy: Still in the “science lab” phase, but researchers are working hard on smarter, more precise drugs.
Radiation Therapy
Radiation isn’t the star player here, but it can help clean up leftover cancer cells or ease pain if the cancer spreads.
Hormone Replacement Therapy
Since the adrenal glands make essential hormones, many patients need lifelong hormone meds after treatment. Think of it as replacing what the body can’t make anymore—totally manageable with the right care.
Clinical Trials
Because this cancer is rare, clinical trials are a big deal. They give patients access to cutting-edge treatments and help doctors discover better cures for the future.
Living with Adrenal Cortex Cancer: Quality of Life Considerations
A diagnosis of adrenal cortex cancer affects not only physical health but also emotional, psychological, and social well-being.
Managing Side Effects
Treatment-related side effects can be significant. Mitotane commonly causes gastrointestinal upset, fatigue, and neurological symptoms. Working closely with your healthcare team to manage these effects is essential for maintaining quality of life.
Hormone Management
Patients who’ve had adrenalectomy or are taking mitotane need careful hormone monitoring and adjustment. This includes:
- Taking prescribed hormone replacement medications consistently
- Carrying an emergency injection of hydrocortisone
- Wearing medical alert identification
- Understanding sick day rules for stress situations
- Regular follow-up with an endocrinologist
Emotional Support
Dealing with a rare cancer diagnosis can feel isolating. Consider:
- Joining support groups (online or in-person)
- Working with a mental health professional
- Connecting with organizations specializing in rare cancers
- Maintaining open communication with family and friends
Follow-Up Care
Regular monitoring is crucial for detecting recurrence. Follow-up typically includes:
- Physical examinations every 3-6 months
- Hormone level monitoring
- Imaging studies (CT or MRI) at regular intervals
- Blood work to assess overall health and medication levels
The Future: Research and Hope
Despite being rare, adrenal cortex cancer continues to be the focus of important research. Scientists are investigating:
- Genomic Studies: Identifying genetic mutations and molecular pathways involved in ACC development may lead to targeted therapies.
- Immunotherapy: Checkpoint inhibitors and other immune-based treatments are being explored for their potential in treating advanced disease.
- Improved Imaging: Advanced imaging techniques may enable earlier detection and better treatment monitoring.
- Novel Drug Combinations: Researchers are testing various medication combinations to improve outcomes for advanced ACC.
- Biomarkers: Developing better biomarkers could help predict treatment response and prognosis.
Conclusion: Knowledge Empowers Action
Here’s the big takeaway: adrenal cortex cancer is rare and scary—but knowing the signs can change everything. Hormone changes plus belly pain aren’t “just random.” When people catch this cancer early, doctors have way more tools to fight it.
If something feels off, speak up. Seriously. I’ve seen early action save lives. And if you or someone you love is diagnosed, know this—you’re not facing it solo. There are expert doctors, better treatments than ever, and real humans who’ve walked this road and are ready to help.