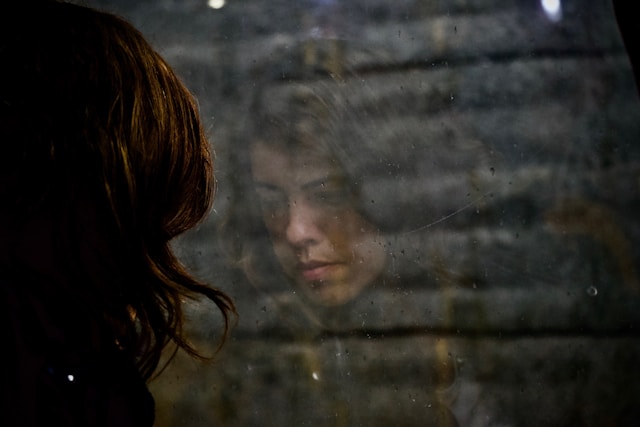
Depression is a mental health condition that impacts millions of people worldwide.
While many see it as just an emotional or psychological issue, it goes far beyond that.
Depression actually affects different parts of the brain, changing how it works.
Understanding how the brain is involved in depression is important because it helps us find better ways to treat it and improve mental health care.
In this article, we’ll look at how the brain plays a role in depression, what happens to the brain during this condition, and how various treatments aim to address these changes.
Importance of Understanding the Brain’s Role in Depression
Depression is a complicated mental health condition influenced by many factors, including life experiences and emotional challenges.
However, the brain’s function plays a major role in how depression develops and affects a person.
By learning about the specific parts of the brain and the chemicals involved, doctors can create more focused treatments and therapies.
This knowledge also helps people with depression and their loved ones better understand the condition, making it easier to manage the symptoms.

Neurological Mechanisms of Depression
Depression impacts the brain in many ways, including changes in its structure and chemical balance.
Let’s break down which parts of the brain are affected and how brain chemicals, called neurotransmitters, play a role.
Brain regions affected
There are a few key areas of the brain that are directly involved in depression:
Prefrontal cortex
This part of the brain helps us make decisions, regulate emotions, and solve problems.
When someone has depression, this region tends to be less active, which makes it harder to manage emotions and think clearly.
This can lead to feeling overwhelmed by even simple tasks.
Amygdala
This is the brain’s emotion center, especially when it comes to fear and pleasure.
In people with depression, the amygdala often becomes overactive, causing them to feel heightened emotional sensitivity.
This can make negative feelings, like sadness or anxiety, much more intense.
Hippocampus
The hippocampus plays a big role in memory and learning.
Depression can actually shrink this part of the brain, which affects how well a person can remember things and process new information.
This is why people with depression often report having trouble concentrating or feeling forgetful.
Neurotransmitters
Neurotransmitters are chemicals that help brain cells communicate with each other.
In people with depression, these chemicals can become imbalanced, leading to various symptoms.
Serotonin
Known as the “feel-good” chemical, serotonin helps regulate mood, sleep, and appetite.
People with depression often have lower levels of serotonin, which can lead to feelings of sadness, poor sleep, and changes in eating habits.
Dopamine
Dopamine is responsible for feelings of pleasure and reward.
When dopamine levels are low, it’s harder to feel motivated or find joy in things that used to be enjoyable.
This is why people with depression often feel apathetic and lose interest in activities they once loved.
Norepinephrine
This chemical helps the brain respond to stress and also affects attention and focus.
When norepinephrine is out of balance, it can cause fatigue and trouble concentrating—two common symptoms of depression.

Brain Changes Associated with Depression
Depression isn’t just about mood swings—it brings tangible changes to the brain’s structure and function.
Reduced gray matter volume in key brain regions
Studies show that individuals with depression often have reduced gray matter volume in regions like the prefrontal cortex and hippocampus.
Gray matter is crucial for processing information, and its reduction can impair cognitive abilities like decision-making and memory.
A study published in The Lancet Psychiatry found that people with recurrent depression had a reduction in gray matter volume compared to healthy individuals.
Altered neural connectivity
In addition to structural changes, depression alters the way brain regions communicate with each other.
Research shows that the connections between the amygdala and the prefrontal cortex become weaker.
This disrupts emotional regulation, leading to more intense negative emotions and difficulty controlling them.
Increased activity in the amygdala
The amygdala is hyperactive in those with depression, especially when processing negative emotions or stressful stimuli.
This overactivity is linked to heightened emotional responses, making it harder for individuals to manage stress or avoid negative thinking patterns.
Decreased activity in the prefrontal cortex
Conversely, the prefrontal cortex, which helps regulate emotions and control impulsive actions, becomes underactive during depression.
This imbalance between an overactive amygdala and an underactive prefrontal cortex explains why people with depression often struggle with emotional regulation and decision-making.

Impact on Cognitive Functions
Depression does more than affect mood—it also impairs cognitive functions like attention, memory, and executive functioning.
Attention and memory problems
Many people with depression struggle to focus, have trouble remembering things, and find it difficult to process information.
These issues are linked to changes in important brain areas like the hippocampus (which helps with memory) and the prefrontal cortex (which helps with attention and decision-making).
Executive functioning difficulties
Executive functions are the mental skills that help us plan, solve problems, and control our impulses.
Depression can seriously impair these abilities, making even simple tasks—like deciding what to eat or paying bills—feel overwhelming.
This struggle adds to the sense of hopelessness that many people with depression experience, because it feels like they can’t cope with everyday life.
Treatment Approaches
Since depression affects both mood and brain function, treating it often requires multiple approaches.
There’s no single cure for depression, but different treatments can target the brain changes and chemical imbalances that come with the condition.
Talk therapy (Psychotherapy)
One of the most common treatments is Cognitive Behavioral Therapy (CBT).
This type of therapy helps people change negative thought patterns and learn better coping strategies.
Interestingly, CBT doesn’t just change how you think—it can also physically change brain activity, particularly in the prefrontal cortex, which is responsible for regulating emotions.
This helps people manage their feelings more effectively.
Medications
Antidepressants, like SSRIs (Selective Serotonin Reuptake Inhibitors), are medications that increase the levels of serotonin—a “feel-good” chemical—in the brain.
By boosting serotonin, these drugs help improve mood and relieve other symptoms of depression.
According to a study from 2020, 50-60% of people with depression experience improvements in their symptoms after taking antidepressants.
Alternative therapies
In addition to traditional treatments, some alternative therapies are gaining attention.
For example:
- Mindfulness meditation: This practice helps people stay grounded in the present and can reduce stress and improve mood.
- Transcranial Magnetic Stimulation (TMS): This is a newer, non-invasive treatment that uses magnetic fields to stimulate the prefrontal cortex, helping regulate mood in people who haven’t responded to other treatments.

Final Thoughts
Depression is not just a mental health issue; it is closely linked to changes in the brain’s structure and how it works.
By understanding these brain changes, we can better grasp the complexity of depression and approach treatment with more care and accuracy.
While we’ve made progress in understanding how the brain is involved in depression, there’s still more to learn.
Ongoing research is essential for creating more personalized and effective treatments in the future.
FAQs
Depression leads to structural changes in the brain, including reduced gray matter volume in key regions like the prefrontal cortex and hippocampus, as well as altered neural connectivity.
In many cases, yes. Treatments such as antidepressants, psychotherapy, and alternative therapies can help normalize brain function and alleviate symptoms.
The prefrontal cortex, amygdala, and hippocampus are among the most affected regions, influencing emotional regulation, memory, and decision-making.
Antidepressants like SSRIs increase the availability of neurotransmitters like serotonin, helping to improve mood and restore balance in brain function.


