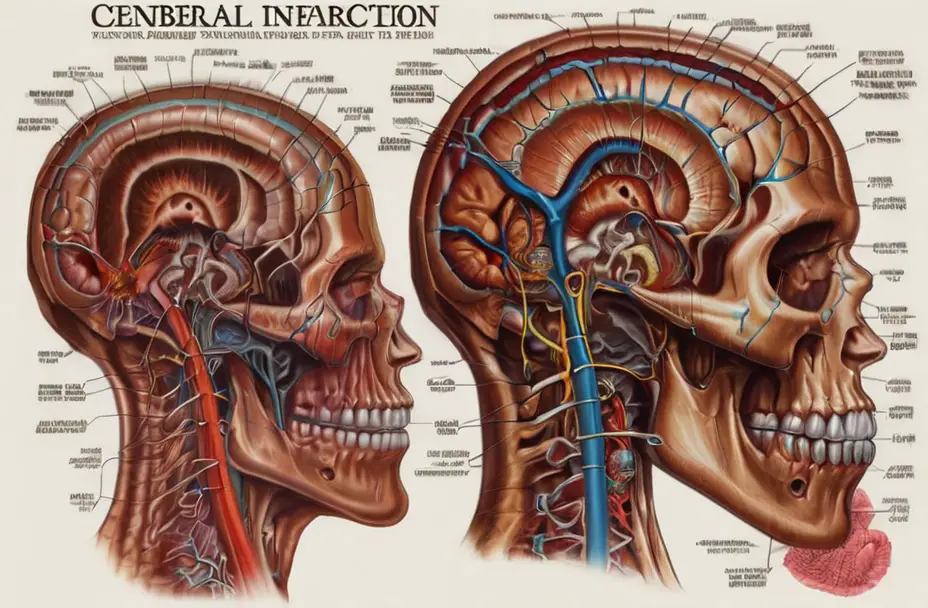
Cerebral infarction, also known as a stroke, is a serious medical condition that occurs when blood flow to a specific area of the brain is disrupted, leading to cell death and potential neurological deficits.
In this blog post, we will discuss the pathophysiology of cerebral infarction, its various classifications, causes, effects, and treatment strategies.
What is Cerebral Infarction
Cerebral infarction occurs when blood flow to a part of the brain is disrupted, leading to the death of brain cells and potential neurological deficits.
There are two main types of cerebral infarction: ischemic and hemorrhagic.
Ischemic cerebral infarction is caused by the blockage of a blood vessel supplying the brain, typically due to a blood clot or an embolus (a foreign substance that travels through the bloodstream and lodges in a blood vessel).
Hemorrhagic cerebral infarction is caused by the rupture of a blood vessel in the brain, leading to bleeding within the brain.
- Read also: Does Strokes Cause Memory Loss: Facts to Know
- Read also: Decoding the Differences: Cerebral Hemorrhage vs. Stroke
Various Classifications of Cerebral Infarction
Cerebral infarction can be classified based on the location of the lesion, the size of the infarct, and the duration of the ischemia.
Some common classifications include:
- Anterior circulation infarction: Affects the frontal and temporal lobes, as well as the internal capsule.
- Posterior circulation infarction: Affects the occipital, temporal, and parietal lobes, as well as the cerebellum and brainstem.
- Lacunar infarction: Small, deep infarcts located in the basal ganglia or internal capsule.
- Watershed infarction: Occurs at the boundaries of blood vessel territories, often due to reduced blood flow to the brain.

Causes of Cerebral Infarction
The causes of cerebral infarction are diverse and can be attributed to various underlying health conditions.
Understanding these primary causes is crucial for prevention and effective management.
Atherosclerosis
Atherosclerosis is a leading cause of cerebral infarction.
It involves the gradual buildup of plaque within the arteries, narrowing the vessels and restricting blood flow.
This plaque can rupture, leading to the formation of blood clots and emboli.
When these clots or emboli travel to the brain, they can block blood vessels, causing ischemic infarction – a lack of blood supply leading to tissue damage.
Hypertension
High blood pressure is a significant risk factor for cerebral infarction.
Prolonged hypertension can weaken the walls of blood vessels, making them more susceptible to rupture.
In cases of hemorrhagic infarction, high blood pressure may contribute to the rupture of blood vessels, leading to bleeding within the brain. This can result in severe damage to brain tissue.
Atrial fibrillation
Atrial fibrillation, characterized by an irregular heartbeat, poses a risk for cerebral infarction.
In this condition, blood clots can form within the atria of the heart.
These clots may break loose and travel to the brain, causing ischemic infarction by blocking blood vessels.
Managing atrial fibrillation is essential in reducing the risk of stroke, often through medications to prevent blood clot formation.
Cardiomyopathy
Cardiomyopathy, a condition where the heart muscle weakens, can contribute to the development of cerebral infarction.
A weakened heart is less efficient at pumping blood, increasing the likelihood of blood clots forming within the heart chambers.
These clots may then travel to the brain, causing ischemic infarction.
Treating and managing cardiomyopathy is crucial for preventing complications such as cerebral infarction.
Coagulopathy
Disorders affecting blood clotting, known as coagulopathies, can lead to both ischemic and hemorrhagic infarction.
Conditions such as hemophilia or excessive anticoagulant use can disrupt the delicate balance of clotting factors, increasing the risk of abnormal blood clot formation.
This, in turn, can result in either blocked blood vessels or bleeding within the brain, contributing to cerebral infarction.

How Cerebral Infarction Affects the Brain
Cerebral infarction can lead to a range of neurological deficits, depending on the location and size of the infarct.
Common symptoms include:
- Hemiparesis: One of the most common effects of cerebral infarction is hemiparesis, which refers to weakness on one side of the body.
- Hemisensory loss: Cerebral infarction can also lead to hemisensory loss, resulting in a diminished or complete loss of sensation on one side of the body.
- Aphasia: This condition can manifest as difficulty speaking, understanding language, or both.
- Visual field deficits: Cerebral infarction can result in visual field deficits, leading to the loss of vision in one or both eyes.
- Gait and coordination problems: Stroke survivors may face gait and coordination problems, affecting their ability to walk and maintain balance.
Potential Effects of Cerebral Infarction
The long-lasting consequences often depend on factors such as the location and size of the infarct, but they can manifest in various ways, affecting both physical and mental well-being.
- Disability: Depending on where the stroke occurs in the brain, cerebral infarction can result in significant disability.
- Depression: It’s not uncommon for stroke survivors to experience depression and anxiety as a result of the life-altering impact of cerebral infarction.
- Cognitive impairment: Cerebral infarction can lead to problems with memory, attention, and executive function.
- Speech and language difficulties: Depending on the location of the infarct, individuals may experience speech and language difficulties, commonly known as aphasia.
- Emotional and behavioral changes: Individuals may exhibit altered emotional responses, such as heightened irritability, mood swings, or emotional lability.
- Challenges in activities of daily living (ADLs): Stroke survivors may face challenges in performing activities of daily living (ADLs), such as dressing, bathing, and eating independently.
Treatment Strategies for Cerebral Infarction
Treatment for cerebral infarction depends on the type and severity of the infarct. Common treatment strategies include:
Thrombolysis
Thrombolysis is a medical intervention aimed at restoring blood flow to the brain by dissolving blood clots.
This approach is particularly relevant in cases of ischemic infarction, where a clot obstructs blood vessels, leading to diminished blood supply.
Medications, such as tissue plasminogen activator (tPA), can be administered intravenously to break down the clot and promote reperfusion.
Anticoagulation
In cases of hemorrhagic infarction, where bleeding occurs within the brain, anticoagulation therapy may be employed.
Anticoagulant medications, such as heparin or warfarin, are utilized to prevent further bleeding and promote the formation of blood clots.
This helps stabilize the condition and reduce the risk of additional hemorrhage.
Rehabilitation
Rehabilitation is a cornerstone of stroke treatment, encompassing physical therapy, occupational therapy, and speech therapy to address various aspects of recovery.
Physical therapy focuses on improving motor skills, strength, and coordination, helping individuals regain mobility and independence.
Medication management
Medications are often prescribed to manage underlying conditions and reduce the risk of recurrent strokes.
For example, medications to control blood pressure, cholesterol levels, and blood sugar are essential components of post-stroke care.
Additionally, antiplatelet agents like aspirin may be prescribed to prevent the formation of blood clots in certain cases.
Lifestyle modifications
Adopting a healthy lifestyle is integral to stroke prevention and management.
This includes maintaining a balanced diet, engaging in regular physical activity, and avoiding tobacco use.
Lifestyle modifications contribute to overall cardiovascular health, reducing the risk of conditions that may lead to cerebral infarction.
Emotional support and counseling
The psychological impact of cerebral infarction cannot be overlooked.
Emotional support and counseling are crucial components of stroke treatment.
Coping with the aftermath of a stroke, adjusting to new challenges, and addressing potential mental health issues, such as depression and anxiety, are essential for holistic recovery.

- Read also: Understanding the Nuances: Cerebral Infarction vs Stroke
- Read also: A Comprehensive Guide: Cerebral Herniation Symptoms
Conclusion
Cerebral infarction is a complex medical condition that can lead to significant neurological deficits.
Understanding the pathophysiology, classifications, causes, effects, and treatment strategies of cerebral infarction is crucial for providing optimal care and support for stroke survivors.
FAQs
Common symptoms include hemiparesis, hemisensory loss, aphasia, visual field deficits, and gait and coordination problems.
Treatment strategies include thrombolysis, anticoagulation, and rehabilitation.
The long-term effects of cerebral infarction can include disability, depression, and cognitive impairment.
Prevention strategies include managing risk factors such as hypertension, atrial fibrillation, and coagulopathy.


