When parents first hear “cancer” and “brain tumor” mentioned together with their child, the end of the world appears.
Medulloblastoma—awful but now more tame brain cancer—is evidence of medicine’s huge progress.
It’s daunting, indeed, but more children now live each year due to more recent treatment and research.
To know what it is and how physicians battle it can dispel some of the fear with optimism.
What Is Medulloblastoma?
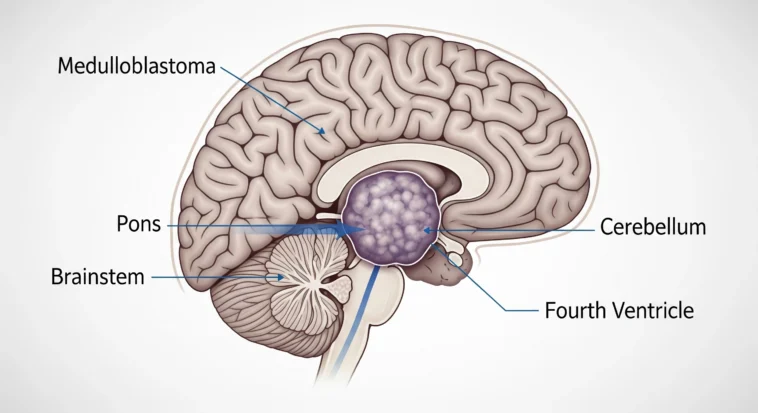
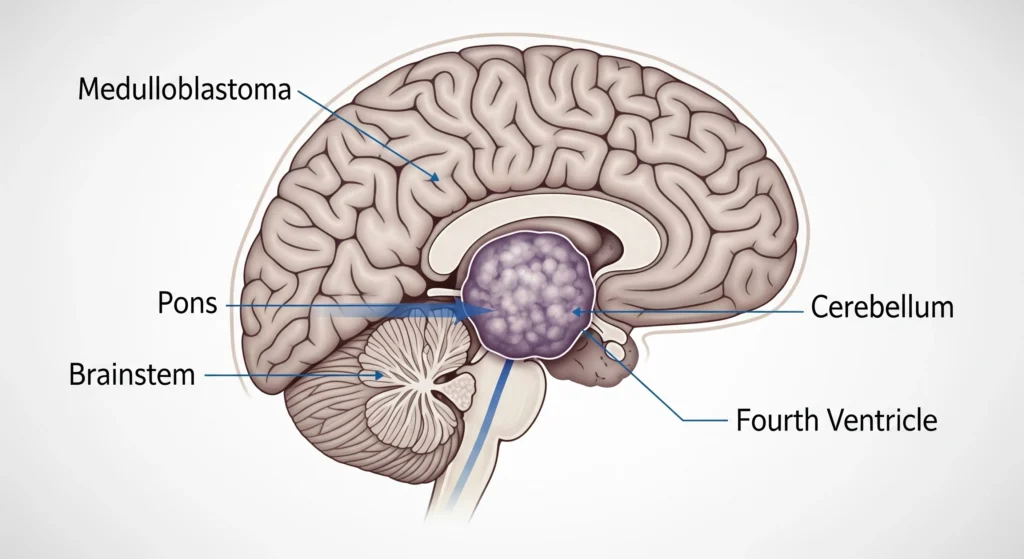
Medulloblastoma is an aggressive, fast-moving tumor that begins in the cerebellum, which is responsible for controlling and supporting your balance and movement.
A neuroepithelial tumor embryonal to stimulate growth in young brain cells during development persists, despite being expected to do so.
This is known as nerdy behavior.
Key characteristics of medulloblastoma include:
- Fast-growing and invasive — it spreads quickly if not treated.
- Likes to hitch a ride in cerebrospinal fluid, so it can travel around the brain and spine.
- Usually lives in the posterior fossa of the cerebellum (that’s the back-bottom part of the skull).
- Has the potential to metastasize to the spinal cord.
It’s the most common malignant brain tumor in kids — making up about 20% of pediatric brain tumors — although it can show up in adults too, most often between about 20 and 45 years old.
Medulloblastoma Statistics
The numbers behind medulloblastoma tell two stories at once: it’s a tough opponent, but it’s also one where medicine is winning more battles every year.
In the U.S., about 435 people are diagnosed each year — and more than 70% of them are kids.
That’s why doctors often call it a “childhood disease,” even though adults can get it too.
Current survival statistics show real hope:
- Around 80% of patients survive 5 years after diagnosis — though this depends on things like age, whether the tumor spread, if it comes back, and the exact subtype.
- With today’s mix of treatments (surgery, radiation, chemo) and smarter ways to sort patients into “risk groups,” long-term survival has jumped to 70–80%.
- Right now, about 6,000 people in the U.S. are living with medulloblastoma.
The odds look different depending on age:
- Kids (0–14 years): about 0.47 per 100,000 are diagnosed each year.
- Teens & young adults: about 0.11 per 100,000.
- Adults over 40: only about 0.02 per 100,000.
Understanding Molecular Subtypes
The recognition of the diversity of tumors in medulloblastoma research has been a significant breakthrough.
The treatment of medulloblastoma by doctors for years was viewed as a single category, with all music being lumped together into one genre without any distinctions.
With the knowledge of four distinct molecular subtypes, scientists have made a significant breakthrough in diagnosing and treating the disease.
The four primary subgroups are WNT, SHH, Group 3, and Group 4. For instance,
The Four Main Molecular Subtypes
WNT (Wingless) Subtype
- Usually comes with the best outlook.
- About 10% of all medulloblastomas fall into this group.
- Tends to affect older kids and adults.
- Responds amazingly well to standard treatments.
SHH (Sonic Hedgehog) Subtype
- Can show up at any age, from babies to adults.
- Makes up about 30% of cases.
- Really exciting because it’s opening the door to “targeted therapies” — treatments designed like a lock-and-key just for this type.
- Prognosis (outcome) can swing widely depending on age and genetic details.
Group 3 (MYC-driven)
- The toughest one — it’s aggressive and often comes with the poorest outcomes.
- Mostly affects infants and very young kids.
- Often spreads (metastasizes) by the time it’s found.
- Linked to very high levels of a cancer-driving gene called MYC.
Group 4
- The most common — around 40% of all cases.
- Usually shows up in school-aged kids.
- Prognosis is somewhere in the middle: not as good as WNT, not as harsh as Group 3.
- Scientists are still unraveling the exact “drivers” behind it, but they’re making progress.
Recognizing the Signs and Symptoms
Early recognition of medulloblastoma symptoms can be crucial for prompt diagnosis and Catching medulloblastoma early can make a huge difference — the sooner doctors know what’s going on, the sooner they can step in.
Since this tumor grows in the cerebellum (the part of your brain that helps with balance and coordination) and often blocks the flow of spinal fluid, most of the warning signs come from pressure building up inside the skull or problems with movement.
Common symptoms include:
- Headaches – Not just “I didn’t drink enough water” headaches. These are often really bad and feel worst in the morning.
- Nausea and vomiting – Especially throwing up in the morning without having the flu or food poisoning.
- Balance and coordination problems – Think tripping, wobbling, or falling a lot, even in situations where you normally wouldn’t.
- Changes in behavior or personality – Irritability, seeming extra tired, or even trouble focusing and remembering things.
- Visual problems – Double vision, or feeling like your eyes just can’t keep up.
- Seizures – Less common here than in some other brain tumors, but still possible.
In babies and very young kids, signs can look a little different:
- Head growing too fast – Parents might notice the head size shooting up quickly.
- Bulging fontanelle – That “soft spot” on top of the baby’s head might bulge.
- Developmental regression – Skills like crawling or babbling suddenly fade.
- Persistent crying or irritability – Not just fussy, but constantly upset in a way that feels “off.”
Here’s the takeaway: if a child suddenly has a mix of these symptoms — especially bad morning headaches with vomiting, or sudden clumsiness — it’s not something to “wait and see.”
Current Treatment Approaches
Modern medulloblastoma treatment is like assembling a skilled team: each player (surgery, chemo, radiation) has a job so the team can win while trying to spare the rest of your life from unnecessary damage.
The plan usually combines maximal safe resection, chemotherapy, and craniospinal irradiation (CSI).
Surgery
Maximal safe resection is the opening play — neurosurgeons try to remove as much of the tumor as they can without damaging the parts of the brain that control important functions.
Think of it like carve-away work on a delicate sculpture: get rid of the cracked bits but don’t chip the fine details.
How much they can remove matters — removing over 90% (gross total resection) usually helps outcomes — but the surgeon’s priority is keeping you working and moving afterward.
Surgical considerations include:
- Tumor location and how close it is to critical brain areas
- Patient age and overall health
- Risk of problems with cerebrospinal fluid (the brain’s plumbing)
- Risk of neurological damage or new deficits
Radiation Therapy
After surgery, doctors want to clean up any tiny tumor cells that might be hiding.
Craniospinal irradiation (CSI) treats the entire brain and spinal cord because medulloblastoma can spread through the spinal fluid.
Radiation has gotten a lot smarter lately:
Proton Beam Therapy
- Delivers radiation very precisely, like a laser scalpel for beams.
- Cuts down damage to healthy tissue — huge for kids whose brains are still growing.
- Lowers the long-term risk of secondary cancers.
Intensity-Modulated Radiation Therapy (IMRT)
- Uses computers to shape the dose around the tumor.
- Helps protect normal brain tissue by customizing where the radiation goes.
Chemotherapy
Where tumor cells are not present, chemotherapy is the body-wide weapon that destroys them.
The drug regimen and dosage are determined by age, the tumor’s molecular subtype, and the severity of its risk.
Common drugs include:
- Vincristine
- Cisplatin or Carboplatin
- Cyclophosphamide
- Etoposide
During risk-adaptive therapy, doctors adjust the treatment to suit individual needs while still managing cancer risks and decreasing unnecessary side effects.
Cutting-Edge Advances
New discoveries are making Medulloblastoma treatment more precise, less harsh, and more hopeful than what it was ten years ago.
However, the current treatments are moving quickly.
The tumor will require targeted targeting rather than more intense blasting in the future.
Targeted Therapies
Some of the coolest advances are targeted therapies — treatments that go after very specific tumor pathways.
For SHH-driven tumors (remember the Sonic Hedgehog subtype?), doctors now have drugs designed to shut down that exact signal.
It’s like switching off the Wi-Fi that the tumor depends on.
SHH Pathway Inhibitors
- Drugs like Vismodegib and Sonidegib zero in on the Sonic Hedgehog pathway.
- They work especially well in SHH-subtype tumors.
- In some cases, they could even mean less intense chemo for patients.
Precision Medicine Approaches
- Instead of “one-size-fits-all,” doctors tailor treatments to each person’s specific genetic mutations.
- This personalization makes therapies more effective and spares patients unnecessary side effects.
- It also helps match patients to the right clinical trials faster.
Immunotherapy and Novel Approaches
Harnessing the immune system is one of the most exciting frontiers.
Imagine reprogramming your body’s own defenders to fight the tumor.
CAR-T Cell Therapy
- Scientists take a patient’s T-cells (a type of immune cell), genetically re-engineer them, and send them back in as cancer assassins.
- Early trials are showing promise.
- Could provide long-lasting protection — like training your immune system to “remember” the enemy.
Tumor Treating Fields (TTFields)
- Uses low-intensity electric fields to mess up tumor cell division.
- Completely non-invasive (no scalpels, no needles).
- Currently being tested in medulloblastoma trials.
Advanced Diagnostics
Sometimes, the hardest part isn’t just treatment — it’s figuring out exactly what kind of tumor you’re up against. Here’s where tech steps in.
Image-based Machine Learning
- Algorithms can now scan MRI images and help predict molecular subtypes.
- This could give doctors key info before surgery, without needing a tissue sample.
- It’s faster, less invasive, and cheaper.
Artificial Intelligence Integration
- AI can analyze MRI scans in ways the human eye can’t.
- Helps with non-invasive tumor classification.
- Makes treatment planning sharper and more personalized.
Living with Medulloblastoma
Surviving the tumor is a large accomplishment — but it is far from over.
Life after medulloblastoma has its own challenges, and understanding what to anticipate makes you and your family prepare for the future.
Late Effects
Cognitive and Learning Issues
- Memory and attention issues — you could forget things or struggle with paying attention in school.
- Slower processing speed — things that were rapid in the past may now take longer.
- Additional academic support can be beneficial — tutoring, IEPs, or accommodations in school can greatly improve things.
- Neuropsychological rehabilitation (consider brain training and learning strategies) can assist in rebuilding skills.
Physical Complications
- Growth delays and developmental delays — certain treatments delay the way your body develops.
- Chemotherapy hearing loss — oops, occasionally lifesaving chemotherapy can do it to ears; tests or hearing aids assist.
- Endocrine disorder — drugs can play havoc with hormones, so physicians will monitor for growth, puberty, and thyroid status.
- Second cancers — low risk years from now, that is why follow-up is needed.
Psychosocial Impact
- Adjustment emotionally is to be anticipated — feeling sad, angry, or anxious is acceptable.
- Family stress and changing dynamics — everyone copes differently; that can strain relationships.
- Peer relationships and fitting in — friends might not understand why things are different now.
- Mental health support — counselors or support groups are not just helpful, they’re often essential.
Survivorship Care
Regular follow-up includes:
- Oncological monitoring — routine scans and labs to watch for anything new.
- Neurological assessments — tracking how the brain and nervous system are doing.
- Cognitive evaluation — tests for learning, memory, and attention so schools can help.
- Endocrine screening — checking hormone levels and growth.
- Psychosocial support — counseling and family therapy to handle the emotional stuff.
Support and Resources: No Family Stands Alone
A medulloblastoma diagnosis hits everyone in the family — but you don’t have to go through it by yourself.
There are lots of groups and people who actually get what you’re facing and can help with information, practical support, and someone to talk to.
Key Organizations are:
- National Brain Tumor Society – Big-picture information, advocacy, and resources for families.
- Medulloblastoma.org – Detailed information almost solely about medulloblastoma and current research.
- Children’s Brain Tumor Foundation – Family-centered resources, education materials, and child activities.
- American Cancer Society – General cancer resources, navigation assistance, and hands-on tools.
Supports Available:
- Medical teams – Pediatric oncologists, specialty nurses, and social workers who break down the science and guide your hand through visits.
- Educational champions – School liaisons and special-ed teams who ensure that school functions for you while in and after treatment.
- Support groups – Other families and teens who have been there — people who get the strange pieces.
- Financial assistance – Grants, money, and programs that can provide assistance with bills, transportation, and treatment expenses.
- Participation in research – Clinical trials and new studies that may provide access to new treatments.
Conclusion: Knowledge, Hope, and Action
Medulloblastoma is tough, but it’s also proof of how far medicine has come.
Thanks to breakthroughs in science, treatments are smarter, and survival rates keep climbing.
The big takeaways? Get care at centers that know brain tumors inside out, use molecular subtyping to guide treatment, and never skip long-term follow-up care — it’s what helps kids not just survive, but live well.