Getting told you’ve got a brain tumor? Yeah, that’s everybody’s idea of a nightmare.
The whole thing can feel like you’re suddenly speaking a new language nobody bothered to teach you.
And meningiomas—honestly, you’d think people would talk about them more, since they’re pretty common, but nope, most folks haven’t even heard the word before it blindsides them or someone they love.
So, let’s actually cut through the medical mumbo jumbo and dig into what meningiomas are, what the heck they do to your body, how you spot ‘em, and what the docs can actually do for you.
What Is a Meningioma Brain Tumor?
A meningioma is a tumor located on the meninges—the layers that wrap around the brain and spinal cord for protection.
Unlike most other brain tumors that start in the brain tissue itself, meningiomas come from the membranes around the brain, and most of these tumors are benign (non-cancerous), which means they grow slowly and do not metastasize (spread).
Main features of meningiomas:
If doctors see brain tumors quite often, the chances are quite good that a good portion of them will be meningiomas—about 36% of all brain tumors and spinal cord tumors each year.
- Usually not serious: More than 90% are Grade I tumors, which is a fancy way of saying that they are slow, chill, and not the “bad guy” type of tumor.
- Slow growth: They are slow to grow (months to years) before you may even notice them causing any problems..
- Location: The really weird (and frustrating) thing is that it depends on where the tumor camps out.
Understanding Meningioma Statistics and Demographics
Meningiomas are generally prevalent across the population in different ways related to demographic location.
Current research continues to highlight meaningful epidemiological patterns related to who is at risk.
Prevalence and Incidence Rates
The estimated prevalence of having pathologically confirmed meningioma is approximately 97.5/100,000 in the United States, with 170,000+ individuals alive with this diagnosis.
In addition to an estimated annual incidence rate of 8.81 per 100,000 person-years, meningioma was the most common primary intracranial tumor or 38.3% of all brain tumors.
Age and Gender Distribution
The median age at the time of diagnosis for meningioma is 66 years of age.
The incidence rate among patients age 40+ is 18.69/100,000.
Women are disproportionately affected, with rates at least 2-3 times higher in women compared to men, particularly during their reproductive years.
Emerging Trends
The increase in the incidence of meningiomas from 2004-2010 is postulated to be a reflection of the increase in the use and reliance on radiologic imaging of the head using CTs and MRIs, causing an increase in diagnoses of previously undiagnosed meningiomas that would not have been, based on neuroimaging before
Recognizing Meningioma Symptoms
Symptoms may differ considerably depending on the location, size, and growth rate of the tumor.
Many small meningiomas are asymptomatic and are diagnosed through imaging obtained for other reasons.
However, larger meningiomas can produce a variety of neurological symptoms.
Common Symptoms by Location
Convexity Meningiomas (Surface of Brain)
- Seizures (often the first symptom)
- Gradual weakness or numbness
- Memory impairment or cognitive changes
- Changes in personality
Skull Base Meningiomas
- Visual difficulties (e.g., double vision, visual field cuts)
- Hearing loss or tinnitus (ringing) in the ears
- Facial numbness or weakness
- Balance problems
Parasagittal Meningiomas (Top of Brain)
- Weakness or difficulty with walking (leg weakness)
- Loss of bladder control (urinary incontinence)
- Cognitive percomoance
General Symptoms
With the increase in meningiomas, they create problems such as increased pressure within their skull, which can cause headaches, nausea, and vomiting.
Headache, weakness or paralysis, reduced vision, and speech difficulties are the most frequently observed symptoms.
Progressive headaches are the most common initial manifestation, and they tend to worsen over several weeks or months.
Diagnosis and Imaging
To diagnose a meningioma, one must usually undergo clinical testing along with neurological assessment and more advanced imaging studies.
Along with identifying the location of each tumor, it can also determine its size and how closely it is associated with the rest of the brain.
Imaging Studies.
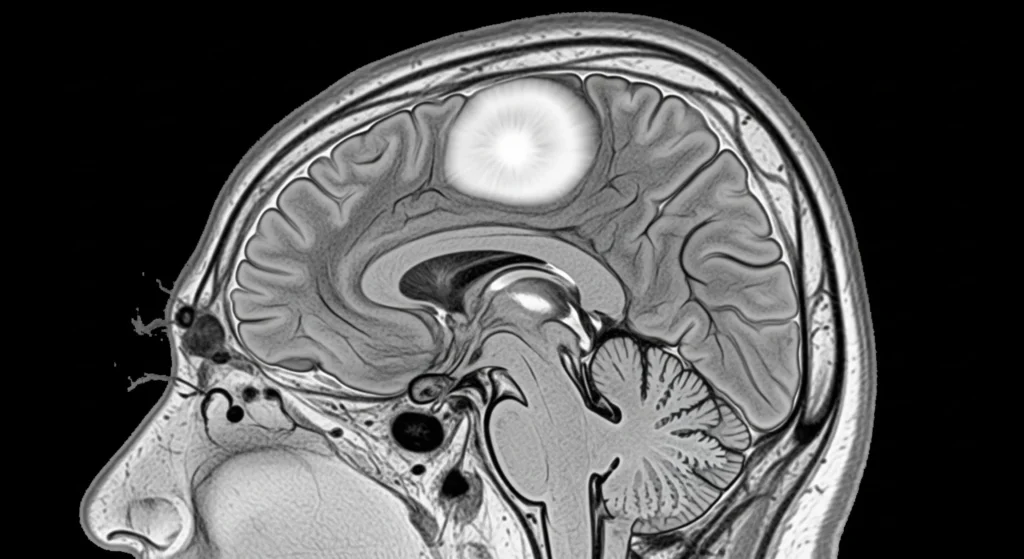
The most reliable method for diagnosing meningioma is through Magnetic Resonance Imaging (MRI).
The contrast enhancement MRI provides detailed information on tumor size, location, and its association with vital brain structures, blood supply patterns, the potential for removal surgery, etc.
During emergency situations, computed tomography (CT) can be used to detect and visualize various types of tumors or fluids, including: early tumor calcification; bone involvement; brain swelling or discharge.
Biopsy and Histological Classification.
Although imaging can provide a preliminary diagnosis, conclusive categorization neceses the examination of tissues. The WHO categorizes meningiomas into three groups:
- Grade I (Benign): Slow-growing tumor with low recurrence risk after complete removal.
- Grade II (Atypical): is an example of aggressive tumor, but with intermediate behavior and higher occurrence rates
- Grade III (Anaplastic/Malignant): meningiomas are aggressive, with a high risk of recurrence and potential for metastasis
Treatment Options for Meningiomas
Figuring out how to treat a meningioma isn’t a one-size-fits-all deal!
Physicians consider the tumor’s size, location, rate of growth, and finally the patient’s age, medical history, and current presenting symptoms.
Active Surveillance
If the tumor is small and it is essentially asymptomatic or very low risk, physicians will not aggressively treat these tumors and may just “watch and wait”.
Active surveillance means:
- Frequent MRIs (more or less every few months up to a year based on stage of tumor, etc.)
- Offices tests of brain and nerve status.
- Monitoring and follow up of any other new active symptoms.
This is commonly utilized in older patients or when surgery would be more risky and not beneficial.
Surgical Treatment
If the tumor is symptomatic and/or increasing in size, surgical intervention is typically the indicated treatment.
The purpose of surgical intervention is to obtain as much of the tumor as possible without compromising surrounding important brain tissue.
- Complete removal – this is obviously preferable – cut it all out – lower chance of tumor recurrence – note, tumors may still come back when gross total is achieved.
- Partial removal – most surgeons will only remove as much as they can without injury – hence, complete removal is not feasible or safe.
Radiation Therapy
Radiation therapy is a critical component of the treatment for meningioma, especially if the tumor was not surgically resected or a recurrent tumor.
Stereotactic Radiosurgery
- Delivers high-dose radiation precisely in a single fraction
- Excellent for treating small to moderate-sized tumors
- Minimal side effects, performed as an outpatient procedure
Fractionated Radiation Therapy
- Delivers many smaller doses over several weeks
- Good choice for prostate tumors or those located near vital structures
- More tolerance for patients with many medical comorbidities
Novel Treatment Approaches
For most patients with atypical and anaplastic meningiomas, additional treatments will follow surgical resection. Treatments may include:
- radiation
- chemotherapy,
- and participating in clinical trials.
Clinical trials typically use novel chemotherapy, targeted therapy, or immunotherapy.
Research continues investigating novel treatment approaches:
- Targeted molecular therapies
- Immunotherapeutic agents
- Advanced radiation delivery modalities
- Hormonal therapies for tumors that are hormone receptor positive.
Prognosis and Long-term Outlook
The good news? The tumor is usually benign (Grade I), and meningiomas are a common occurrence. However, the results can vary depending on certain important factors.
Factors Affecting Prognosis.
- Tumor Grade: Grade I tumors have a survival rate of over 95% after 5 years. Those in the second level are more likely to come back, while those in Grade III are tougher and more aggressive.
- Surgery Success: Surgical procedures with complete tumor removal have minimal chances of success. Leave some, and it will grow again.
- Age & Health: The correlation between age and health is often present, as younger patients tend to recover faster, similar to how athletes recover from an injury.
- Tumor Location: Tumors that are buried near the brain’s critical regions result in increased complexity.
Quality of Life Considerations.
Most patients experience a return to their regular or almost regular lives.
Where the tumor was found, some people may have to handle:
- Ongoing nerve or movement problems.
- The thinking or memory function undergoes changes, especially in larger tumors.
- Seizures that need medicine.
- Unpleasure or fluctuating emotions during recuperation.
When to Seek Medical Attention
A person with a meningiomaumatic condition may find it essential to seek immediate medical assistance at the appropriate time.
While most symptoms develop gradually, certain warning signs resemble flashing red lights, so they should be taken into account before being ignored.
Emergency Warning Signs.
If you notice anything, seek immediate medical attention:
- This is a sudden, hard head pain that feels like nothing you’ve ever experienced before.
- An unexpected feeling of weakness or numbness, such as one side of the body becoming unresponsive.
- A seizure, especially if it’s the first time someone has had one.
- Your vision may suddenly become blurry or double-focused, indicating that your eyes might not be working correctly.
- In the event of sudden confusion or sudden personality changes,
- Unrelenting discomfort or vomiting that persists throughout the day.
Regular Monitoring Signs.
Even though they are not emergency situations, it is crucial to discuss them with your physician:
- Old symptoms slowly getting worse.
- New brain or nerve-related problems becoming more frequent.
- Alterations in pattern or frequency of seizures.
- Symptoms caused by unresponsiveness to medication.
Conclusion: Moving Forward with Knowledge and Hope
Let’s get real for a sec—yeah, “tumor” sounds like a total horror-movie word. Brings the drama, right?
But honestly, meningiomas? They’re usually the chill, slowpoke cousins of the tumor family—super treatable, not out to ruin your life.
Docs these days? Absolute wizards with their tools. Odds are, you’re gonna be just fine.
Biggest thing? Don’t go lone wolf.
Team up with your medical crew, bug them with questions, figure out your options.
Seriously, no shame in hounding them—this is your brain, after all.
Most folks bounce right back to their normal stuff—work, school, binging Netflix, whatever—without missing a beat.



