When someone hears “brain tumor,” it’s totally normal to wonder, “Did this come from my family?” The honest answer is: usually, no. And that surprises a lot of people.
I’ve seen families panic, digging through their family tree like detectives, only to learn that most brain tumors don’t work that way.
Here’s the key idea—genetic doesn’t always mean inherited. Think of your DNA like a massive instruction book. Sometimes, a typo sneaks in over time.
That typo is genetic, but it wasn’t passed down from your parents.
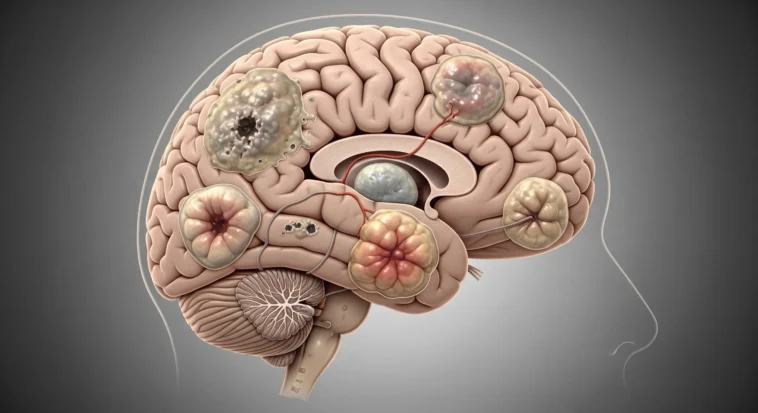
Understanding the Genetic Basis of Brain Tumors
Brain tumors start when brain cells grow out of control because of genetic mutations. These mutations come in two types:
- Germline mutations are the rare ones you’re born with—passed down from parents and present in every cell.
- Somatic mutations are way more common. They happen during your life, in just some cells, often randomly, like a glitch in the system.
Here’s the big takeaway: about 90–95% of brain tumors happen because of somatic mutations, not inherited ones.
That means most people with brain tumors didn’t get it from their parents—and won’t pass it on to their kids. It’s not fate. It’s biology being messy, unpredictable, and sometimes unfair.
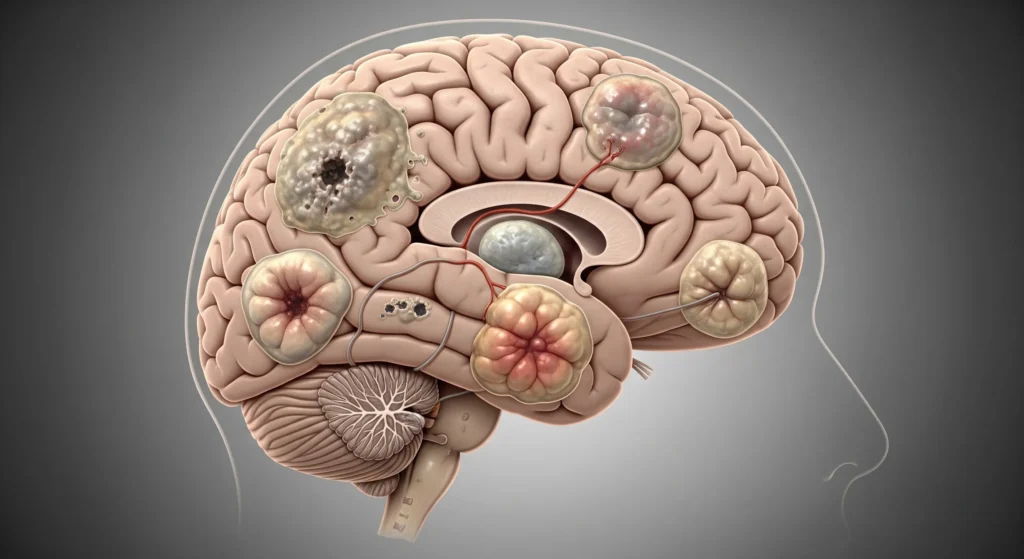
Hereditary Syndromes Associated with Brain Tumors
Okay, quick reality check first: most brain tumors are notinherited. But—plot twist—there are a few rare genetic conditions where brain tumors show up way more often.
These syndromes are caused by germline mutations, meaning you’re born with them, and yes, they can run in families.
Neurofibromatosis Type 1 and Type 2
Think of these as genetic conditions that mess with nerve cells.
- NF1 can lead to tumors like optic gliomas that affect vision.
- NF2 is rarer but famous for causing tumors on both sides of the brain that mess with hearing and balance.
Not subtle. Doctors usually catch these early because symptoms show up young.
Li-Fraumeni Syndrome
This one’s intense. It’s caused by a broken version of the TP53 “tumor police” gene. Without it, cancers—including brain tumors—can pop up early and often.
Families with Li-Fraumeni sometimes have a scary pattern of multiple cancers at young ages.
Tuberous Sclerosis Complex
TSC causes non-cancerous tumors in different organs, including the brain.
The most common brain tumors here grow slowly, and sometimes doctors just watch them instead of rushing into treatment. Not every tumor is a ticking time bomb.
Von Hippel-Lindau Disease
VHL is all about tumors made of blood vessels. In the brain and spine, these are called hemangioblastomas.
People with VHL get regular MRIs—kind of like routine maintenance checks—to catch problems early.
Lynch Syndrome
Usually linked to colon cancer, but surprise—it can also raise the risk of glioblastoma, a serious brain cancer. A rare version called Turcot syndrome has an even stronger brain tumor connection.
Family History and Relative Risk
Let’s talk about family history—because this part sounds scarier than it usually is.
Imagine two kids standing in the rain. One has an umbrella, one doesn’t. Yes, one gets wetter faster—but we’re still talking about rain, not a hurricane.
If you have a close family member (like a parent, sibling, or child) who’s had a brain tumor, your risk is about twice as high as average. That sounds huge… until you zoom out.
Brain tumors are rare to begin with—around 6 out of 100,000 people each year. Double a tiny number and it’s still tiny.
Also, that family connection doesn’t automatically mean “bad genes.” Families share environments, habits, and sometimes just plain bad luck. Most of the time, there isn’t a single inherited mutation hiding in the family tree.
The Role of Genetic Testing
Now, this is where science gets kind of cool. Genetic testing is like running your DNA through a high-powered scanner—but it’s only useful in certain situations.
Doctors might suggest genetic testing if:
- Several family members have had brain tumors or related cancers
- Someone gets a brain tumor really young
- One person develops more than one tumor
- There are physical clues linked to genetic syndromes
- A known cancer-related gene mutation already exists in the family
The test itself is simple—usually blood or saliva. The hard part? Understanding the results. That’s why genetic counseling matters.
A counselor helps explain what the results actually mean, what they don’t mean, and how to deal with the emotional weight that can come with knowing your genetic risk.
Environmental Factors and Gene Interactions
Think of your genes like a loaded app on your phone—and the environment is what taps “open.” Genetics sets the stage, but environmental triggers decide what actually happens.
- Ionizing radiation: High-dose radiation exposure, particularly during childhood, is the most clearly established environmental risk factor for brain tumors.
- Chemical exposures: Certain occupational exposures and chemicals are under investigation, though evidence remains less conclusive than for radiation.
- Immune system factors: Immunosuppression and certain viral infections may play a role in some brain tumor types.
If someone already has a genetic vulnerability, these environmental factors can act like gasoline on a spark—not guaranteed, but riskier.
Recent Research and Future Directions
Here’s the hopeful part. Science is moving fast. Researchers have found lots of tiny genetic changes that each nudge risk just a little. Alone, they’re weak—but together, they can explain why brain tumors sometimes run in families.
They’re also studying epigenetics, which is basically how life experiences turn genes on or off without changing the DNA itself. Wild, right?
And best of all? Precision medicine is becoming real. Doctors can now match a tumor’s exact genetic glitch with treatments designed just for it.
The future of brain tumor care isn’t one-size-fits-all—it’s personal, smarter, and getting better every year.
What This Means for You and Your Family
If brain tumors are something you’re worried about, take a breath—you’re not powerless here. I’ve seen families go from anxious and overwhelmed to calm and confident just by taking a few smart steps.
Discuss Your Family History
Talk to a doctor and be honest—don’t play medical trivia night from memory. Write things down: who had cancer, what kind, and how old they were.
These details help doctors decide if genetic counseling or testing even makes sense for you.
Stay Informed
If your family has a known genetic risk, doctors may suggest regular checkups or scans. Catching things early can make a huge difference. Knowledge here isn’t scary—it’s protective.
Maintain a Healthy Lifestyle
This isn’t a magic shield, but it matters. Eat well, sleep, move your body. Just know this: most brain tumors aren’t caused by anything you did wrong.
This is about stacking the odds in your favor, not blaming yourself.
Seek Support
You don’t have to figure this out alone. Patient advocacy groups are packed with people who get it—they share real stories, real advice, and help fund research that’s saving lives.
Conclusion
So—are brain tumors genetic? The real answer is “sometimes, but usually not.” Most brain tumors happen because of random genetic glitches, not because something was passed down through your family. Still, genetics does matter.
A small number of cases are linked to inherited syndromes, and having a family history can nudge the risk up a bit.
Here’s the exciting part: science is getting really good at reading the genetic “fingerprints” of tumors. That means better early detection, smarter monitoring, and treatments designed for your specific tumor—not some generic checklist.