Traumatic brain injury (TBI) is way more serious than most people realize.
You might bounce back from a concussion in a week and think you’re fine—but years later, memory problems or sudden anger can show up out of nowhere.
I’ve seen it happen to patients who thought they were “all better” after a car accident.
It’s like a tiny crack in a building’s foundation—looks okay at first, but over time, the whole structure weakens. That’s why taking care of your brain isn’t just smart—it’s non-negotiable.
What Is Traumatic Brain Injury?
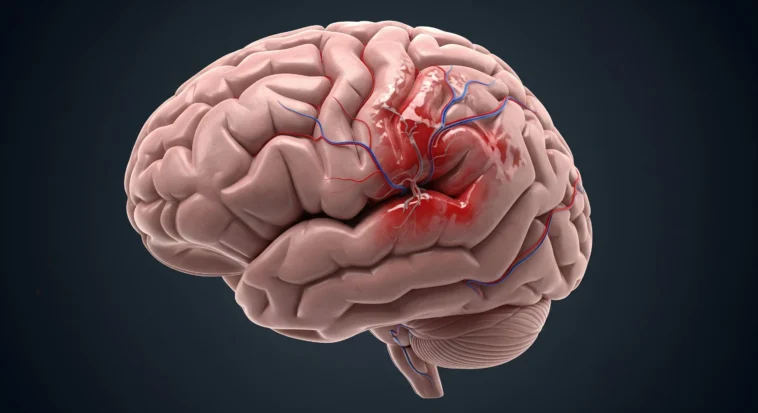
A traumatic brain injury (TBI) happens when your brain gets hurt by an outside force—like a hard hit, a nasty fall, or even something sharp entering the skull.
It’s not like breaking an arm, where you slap on a cast and know it’ll heal in a few weeks.
The brain is trickier.
After the hit, the effects can keep unfolding for months—or even years—like a ripple spreading out long after you drop a stone in water.
Types and Severity of TBI
Doctors usually group TBIs into three levels:
Mild TBI (Concussion)
- You might black out for just a few seconds—or not at all. Sometimes it’s more like feeling dazed or “out of it.”
- Headaches, brain fog, or forgetting where you put your phone five times in a row? Classic signs.
- The tough part? You often look fine, so people around you may not get how real the injury is.
Moderate TBI
- This is more serious. We’re talking about being knocked out anywhere from half an hour to almost a full day.
- Think major memory issues, trouble concentrating, or feeling like your brain is running on low battery.
- Usually, you’ll end up in the hospital, with doctors keeping a close eye.
Severe TBI
- This is the big one: coma or being unconscious for more than a day.
- It can change everything—thinking, moving, even basic daily life.
- Recovery often takes a whole medical team and long-term care.
Common Causes of Traumatic Brain Injury
TBI can sneak up in everyday life, not just in extreme situations:
- Car accidents – the #1 culprit. I once had a patient who thought a “fender bender” was no big deal—until memory problems showed up later.
- Falls – especially dangerous for older people. A simple trip on the stairs can do serious damage.
- Sports hits – football tackles, soccer headers, even skateboarding wipeouts.
- Violence – assaults or physical fights.
- Military combat – explosions and blasts carry massive force.
- Workplace accidents – especially in construction or heavy labor jobs.
Comprehensive Overview of Long-Term Neurological Effects
Cognitive impairments
Okay, think of your brain like the ultimate computer.
After a TBI, the “software” can start glitching—and it’s way more than just misplacing your phone.
Memory problems
It’s like your brain’s save button broke.
You might sit through a movie, laugh at all the jokes, and an hour later it’s like it never happened.
Or maybe a whole piece of your past is just… gone, like someone hit delete.
Executive function deficits
This is your brain’s CEO—the boss that makes decisions, sets plans, and keeps everything running.
After a TBI? The boss might be on vacation.
Choosing what to eat can feel like solving a math test, planning a project is overwhelming, and multitasking?
Forget it—your brain just “blue screens.”
Sometimes you know the answer to a problem, but your mind won’t connect the dots.
Processing speed and attention issues
Imagine everyone else is zipping along on 5G, and you’re stuck on dial-up.
Conversations blur, your focus slips, and every little distraction pulls you off course.
Even thinking hard for a while can leave you so drained you need a nap.
It’s like your brain keeps saying, “Hold on, still loading…”
Emotional and behavioral changes
This one can be the hardest, because it changes how people see you.
A TBI can literally rewire your emotions.
It’s not about being “moody”—the circuits that control feelings got scrambled.
Mood disorders
Think of the worst day you’ve ever had, then imagine being stuck in that mood for weeks or months.
That’s depression after TBI.
Or picture anxiety swooping in out of nowhere—your heart racing for no reason.
Emotions get stuck on high alert, and someone can go from calm to furious over the smallest thing.
Behavioral modifications
Here’s where it gets rough.
The brain’s “filter” that usually says, “Hey, maybe don’t say that”? Sometimes it just shuts off.
I’ve seen kind, gentle people suddenly curse like sailors or explode over something tiny, like spilling a drink.
It’s not “them being mean.” It’s their injury talking.
Social and interpersonal difficulties
This can make people feel super isolated.
They might miss sarcasm, say the wrong thing, or just not read the room anymore.
Imagine being funny before and now your jokes always land flat—it’s heartbreaking.
Friends sometimes drift away, not realizing it’s the injury, not the person.
Physical neurological consequences
And it’s not just thoughts or feelings—the body can get hijacked, too.
Motor function impairments
Think of trying to play your favorite video game, but the controller is lagging and one button won’t work.
That’s what movement can feel like.
A leg might drag, hands fumble with buttons on a shirt, balance wobbles.
It’s your own body refusing to cooperate.
Sensory disturbances
The world can turn into sensory chaos.
Lights feel blinding, normal voices sound like shouting, and even smells can vanish.
Imagine living in constant sensory overload.
Sleep and circadian rhythm disruptions
This one’s sneaky but brutal. After a TBI, your body clock can go haywire.
You’re dead tired but wide awake at 3 a.m., or you sleep 12 hours and still feel like a zombie.
Without good sleep, healing slows way down—but the brain won’t cooperate. It’s like your sleep app is permanently broken.
The Growing Link Between TBI and Neurodegenerative Diseases
Research now shows that a brain injury doesn’t just mess you up in the moment—it can set you up for serious problems years later, like dementia.
This changes how we think about recovery and even how we prevent brain diseases.
TBI and dementia risk
If you’ve had a moderate or severe TBI, your chances of developing dementia later go up 2 to 4 times compared to someone who hasn’t.
One big study found TBI raises dementia risk by about 70%, especially in young men and Asians.
And here’s the kicker—people with 2 or more TBIs saw their brainpower decline twice as fast as those without injuries.
Mechanisms of neurodegeneration
So why does this happen? A few culprits:
- Protein buildup – TBIs can trigger the same bad proteins seen in Alzheimer’s.
- Chronic inflammation – the brain stays “angry” for years, slowly damaging itself.
- Broken wiring – TBI can snap the brain’s white matter “cables,” making aging hit harder.
Alzheimer’s disease and TBI
Doctors now see TBI as a possible fast-forward button for Alzheimer’s.
Not everyone with a TBI gets it—but for some, the clock starts ticking earlier.
That’s why protecting your brain now isn’t just about today—it’s about the next 50 years.
Secondary Complications and Comorbid Conditions
A brain injury doesn’t just stop at the injury itself—it can open the door to other problems that show up later and make life even harder.
Seizure disorders
Around 1 in 10 people with a TBI end up with seizures, especially after a really bad injury.
These can show up right away (in the first week), later on, or turn into full-blown epilepsy with repeated seizures.
Neuroendocrine dysfunction
Your brain also controls your hormones, and TBI can scramble that system.
Things like growth hormone, thyroid, stress hormones, and even reproductive hormones can all go haywire.
Psychiatric complications
This one’s huge. Depression, anxiety, PTSD, even substance abuse can creep in after a TBI because the brain’s chemistry gets rewired.
And it’s not about “being weak”—it’s the injury itself.
Risk Factors for Long-Term Complications
Not everyone with a brain injury ends up with the same long-term problems—it depends on a mix of factors.
Injury-related factors
The bigger the hit, the higher the risk.
Severe injuries, bleeding in the brain, or being knocked out for a long time all make things worse.
Individual factors
Age matters—a lot. Both young brains and older brains are more vulnerable.
Pre-existing issues like depression or epilepsy can stack the odds, and even your genes can tilt the scale.
Plus, if you’re already in rough health, recovery gets tougher.
Environmental and social factors
It’s not just biology.
If you get great medical care, have supportive friends and family, and a stable lifestyle, your chances improve.
On the flip side, stress from school, work, or substance use can drag recovery down.
Treatment and Management Strategies
Treating a brain injury isn’t just about surviving the hit—it’s about healing over the long haul.
Acute phase management
Right after the injury, doctors focus on keeping you alive and stable: protecting your breathing, reducing brain pressure, and stopping more damage.
It’s like putting out the fire before rebuilding the house.
Long-term rehabilitation
This is where the real work begins.
- Cognitive rehab – training your memory, focus, and problem-solving. I’ve seen teens use apps and games to retrain their brains, like brain “workouts.”
- Physical therapy – rebuilding strength, balance, and coordination so you can move without your body fighting back.
- Occupational therapy – relearning everyday stuff: cooking, schoolwork, even job skills. Sometimes it’s about finding new hacks to get around limits.
- Speech & language therapy – not just for talking, but also swallowing, thinking clearly, and handling social conversations again.
Medical management
Doctors also treat specific symptoms—like meds for seizures, depression, or sleep.
Hormone therapy can help if the brain messes with your endocrine system.
And researchers are testing new treatments to protect the brain from long-term damage.
Prevention and Risk Reduction
The best way to deal with a brain injury? Don’t get one in the first place.
Protecting your head is way easier than trying to fix it later.
Primary prevention
- Safety gear – Helmets, seatbelts—yeah, they might not look “cool,” but they save lives. I’ve seen skateboarders walk away from nasty crashes just because they wore a helmet.
- Fall prevention – Especially important for older folks—simple fixes at home can prevent devastating injuries.
- Sports safety – Rules and good coaching aren’t just “boring” regulations—they keep players safe.
- Workplace safety – Hard hats and safety checks exist for a reason.
- Public health programs – Things like traffic safety ads, anti-violence campaigns, and building codes all quietly save thousands of brains every year.
Secondary prevention
- Spot it early – If you hit your head, don’t brush it off. Get checked.
- Concussion protocols – Rest and recover properly—going back too soon risks making things way worse.
- Prevent repeat injuries – One TBI is bad, but a second one before you’re healed? That’s when long-term damage skyrockets.
- Long-term checkups – Doctors can catch problems early before they snowball.
Conclusion
Traumatic brain injury isn’t just a “one and done” problem—it’s one of the toughest medical challenges out there.
We now know TBI isn’t only about what happens right after the hit—it can become a chronic condition that changes your life years down the road, even raising your risk for dementia.
The effects aren’t just physical.
They can mess with your memory, mood, friendships, school, work—you name it.