Cytotoxic cerebral edema (CE) is a serious condition that can lead to brain swelling and potentially life-threatening complications.
In this blog post, we’ll discuss what cytotoxic edema is, how it differs from other types of brain swelling, common causes, warning signs and symptoms, diagnosis, treatment, and answer some frequently asked questions.
What is Cytotoxic Edema?
Cytotoxic edema is a form of brain swelling known as cerebral edema.
It happens when there’s a disturbance in the blood-brain barrier, which normally regulates fluid balance in the brain.
This disruption allows fluid to build up in the brain, creating pressure and possibly severe complications that threaten life.
How Does Cytotoxic Edema Differ from Other Types of Brain Swelling?
Cytotoxic edema sets itself apart from other forms of brain swelling like vasogenic edema.
While vasogenic edema results from increased blood flow, cytotoxic edema arises due to a disruption in the blood-brain barrier.
This crucial difference distinguishes the two conditions in terms of their underlying causes and mechanisms.

Common Causes of Cytotoxic Edema
Cytotoxic edema, a type of brain swelling, can stem from various sources:
Infections
Infections caused by bacteria, viruses, or fungi can compromise the integrity of the blood-brain barrier, leading to cytotoxic edema.
When pathogens invade the brain, they trigger an inflammatory response that disrupts the normal functioning of the barrier, allowing fluid to accumulate in the brain tissue.
Toxins
Exposure to certain toxins, such as heavy metals or chemicals, can induce cytotoxic edema.
These toxins may directly damage the blood-brain barrier, causing it to become leaky and allowing fluid to seep into the brain.
Prolonged or high-level exposure to toxins can exacerbate this effect, resulting in significant brain swelling.
Drugs
Some medications, including corticosteroids, have been linked to cytotoxic edema.
These drugs can alter the permeability of the blood-brain barrier, making it more susceptible to fluid leakage.
As a result, fluid accumulates in the brain, leading to edema.
It’s essential for healthcare providers to monitor patients closely for signs of cytotoxic edema when prescribing medications known to affect the blood-brain barrier.
Trauma
Head injuries or other types of trauma can cause cytotoxic edema by directly damaging the blood-brain barrier.
The force of impact can disrupt the integrity of the barrier, allowing fluid to leak into the brain tissue.
This type of edema is often seen in cases of traumatic brain injury and can have serious implications for neurological function.

Warning Signs and Symptoms of Cytotoxic Edema
Cytotoxic edema is a type of cerebral edema that occurs when cells in the brain swell due to a disruption in the blood-brain barrier.
This can lead to a buildup of fluid within the brain, which can cause pressure and potentially life-threatening complications.
Here are some of the warning signs and symptoms of cytotoxic edema:
- Headache: A severe, persistent headache is one of the most common symptoms of cytotoxic edema.
- Nausea and vomiting: Nausea and vomiting can also be signs of cytotoxic edema.
- Seizures: Seizures can occur in severe cases of cytotoxic edema.
- Loss of consciousness: In severe cases, cytotoxic edema can cause loss of consciousness.
- Focal neurological deficits: Depending on the location of the cytotoxic edema, there may be specific neurological symptoms, such as weakness, numbness, or vision changes.
- Papilledema: This is a swelling of the optic nerve head, which can be a sign of increased intracranial pressure.
- Increased intracranial pressure: Cytotoxic edema can lead to increased intracranial pressure, which can cause a variety of symptoms, including headache, nausea, vomiting, and altered mental status.
- Altered mental status: In severe cases, cytotoxic edema can cause altered mental status, ranging from confusion to coma.
Diagnosis and Treatment of Cytotoxic Edema
Cytotoxic edema is a serious condition that can lead to brain swelling and potentially life-threatening complications.
Here’s how it is diagnosed and treated:
Diagnosis
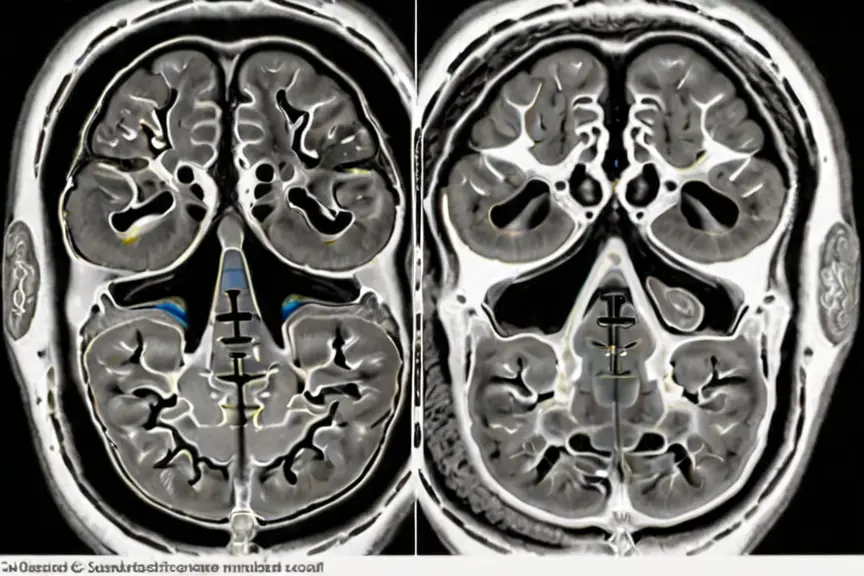
Imaging techniques
- CT Scan (Computed Tomography): A non-invasive scan using X-rays to create detailed cross-sectional images of the brain.
- MRI (Magnetic Resonance Imaging): This technique uses strong magnetic fields and radio waves to produce detailed images of the brain, offering superior visualization of soft tissues like the brain and potentially pinpointing the cause of the edema.
Neurological examination
A doctor will assess your mental status, reflexes, coordination, and other neurological functions to identify potential deficits caused by the edema.
Treatment
Treatment for cytotoxic edema is aimed at addressing its underlying causes. Here’s how it may be approached:
Trauma management
In cases where cytotoxic edema is triggered by trauma, immediate attention is given to treating head injuries or skull fractures.
This involves stabilizing the patient, controlling bleeding if present, and preventing further damage to the brain tissue.
Surgical interventions may be necessary to repair fractures or remove any foreign objects that could exacerbate swelling.
Bleeding control
If cytotoxic edema is associated with bleeding within the brain, prompt measures are taken to manage the hemorrhage.
This typically involves surgical intervention to stop the bleeding and alleviate pressure on the brain.
Medications may also be administered to prevent clot formation and promote blood flow to affected areas.

Ischemia or Hypoxia Management
In cases where cytotoxic edema occurs due to ischemia (restricted blood flow) or hypoxia (low oxygen levels), restoring adequate oxygen supply to the brain is crucial.
This may involve interventions such as administering supplemental oxygen, improving circulation through medications or procedures, and addressing any underlying conditions contributing to reduced oxygen delivery.
Toxic exposures
If cytotoxic edema is caused by exposure to toxins, the primary focus is on removing the toxic substance from the body and minimizing further exposure.
This may involve supportive measures such as administering antidotes, performing gastric lavage or activated charcoal administration to absorb toxins, and providing supportive care to address any complications arising from toxin exposure.
Conclusion
Cytotoxic cerebral edema is a critical condition that can result in brain swelling and severe complications.
Recognizing the warning signs and symptoms is crucial, and it’s essential to seek medical help promptly if you suspect someone you care about may be affected by cytotoxic edema.
FAQs
The prognosis for cytotoxic edema depends on the underlying cause and severity of the condition. Early diagnosis and treatment can improve outcomes.
In some cases, cytotoxic edema can be prevented by avoiding exposure to toxins or discontinuing medications that may cause the condition.
Cytotoxic edema is caused by a disruption in the blood-brain barrier, while vasogenic edema is caused by an increase in blood flow.
The exact prevalence of cytotoxic edema is not known, but it is a serious condition that can lead to life-threatening complications.


