
Depression doesn’t just affect adults—it can impact children, too.
While it’s normal for children to experience sadness from time to time, prolonged periods of intense sadness, irritability, or withdrawal might signal something deeper, such as depression.
Identifying depression early on and seeking help is critical for a child’s emotional and mental well-being.
In this blog, we will explore the common types of depression in children, signs to watch out for, causes, and available treatment options.
Common Types of Depression in Children
Several forms of depression can manifest in children. Here are the most common types:
Major Depressive Disorder (MDD)
Major Depressive Disorder is characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities.
Children with MDD may experience changes in sleep patterns, appetite, and overall energy levels.
According to the Journal of the American Academy of Child and Adolescent Psychiatry, about 3% of children and 6% of adolescents experience MDD annually.
Persistent Depressive Disorder (Dysthymia)
Also known as dysthymia, this type of depression is chronic but less severe than MDD.
Children with dysthymia may feel down for most of the day, nearly every day, for at least one year.
While they may not exhibit intense depressive episodes like those with MDD, the ongoing sadness can interfere with their daily lives.

Bipolar Disorder
Bipolar disorder in children involves extreme mood swings, including episodes of both depression and mania.
The depressive phase can resemble MDD, while the manic phase may involve impulsivity, hyperactivity, and grandiose thinking.
While less common, Pediatrics reports that bipolar disorder often appears in adolescence, though symptoms may be seen in younger children.
Seasonal Affective Disorder (SAD)
Seasonal Affective Disorder (SAD) is a type of depression that typically occurs during the darker months of the year when there is less sunlight.
Children with SAD may feel more tired, irritable, or withdrawn during the winter months and return to their usual selves in the spring and summer.
Research published in Child and Adolescent Mental Health notes that children in regions with shorter daylight periods are more susceptible to SAD.
Adjustment Disorder with Depressed Mood
This type of depression occurs after a child experiences a significant life change, such as the death of a loved one, divorce, or moving to a new city.
Adjustment disorder typically appears within three months of the stressful event and lasts no longer than six months.
Children may struggle with overwhelming sadness, anxiety, or difficulty adapting to their new circumstances.
Cyclothymic Disorder
Cyclothymic disorder is a milder form of bipolar disorder that involves periods of depressive symptoms and hypomanic episodes.
Although the symptoms are less severe, children with cyclothymia may struggle with mood instability, leading to challenges in school and social interactions.
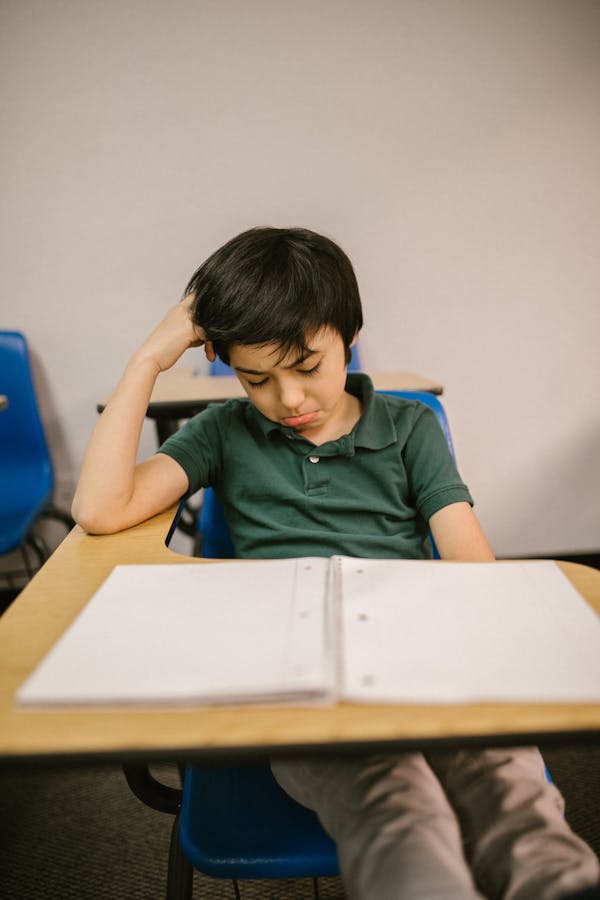
Signs and Symptoms of Childhood Depression
Children with depression may exhibit a wide range of symptoms.
These symptoms are often categorized into four areas: behavioral, emotional, cognitive, and physical changes.
Behavioral changes
- Withdrawal from family and friends
- Loss of interest in previously enjoyed activities
- Sudden changes in sleep or eating habits
- Decline in school performance
- Aggressive or defiant behavior
Emotional changes
- Persistent sadness or hopelessness
- Irritability or anger
- Increased sensitivity to rejection or failure
- Feelings of worthlessness or guilt
- Excessive crying
Cognitive changes
- Difficulty concentrating or making decisions
- Negative thinking patterns
- Frequent thoughts of death or suicide
- Forgetfulness or lack of focus
Physical changes
- Unexplained aches and pains
- Chronic fatigue or lack of energy
- Significant weight loss or gain
- Complaints of stomachaches or headaches without a clear cause

Causes of Depression in Children
Depression in children usually results from a mix of different factors.
Here are some key contributors:
Biological factors
Children with a family history of depression or other mood disorders are more likely to develop depression themselves.
Additionally, imbalances in brain chemicals (neurotransmitters) such as serotonin and dopamine can play a role.
Environmental factors
A child’s environment, including their home, school, and social surroundings, can impact their mental health.
Stressful life events like parental divorce, moving, or family financial difficulties can trigger depressive episodes.
Psychological factors
Children who experience low self-esteem, perfectionism, or feelings of inadequacy are at a higher risk for depression.
These traits can lead to feelings of worthlessness and hopelessness, especially when faced with challenges.
Social factors
Peer relationships can have a profound impact on a child’s mental health.
Bullying, social isolation, or difficulty fitting in with peers can all contribute to feelings of sadness or rejection.
Studies published in The Lancet Child & Adolescent Health show a strong link between bullying and the onset of depressive symptoms in children.

Treatment Options
Depression in children is treatable.
Early intervention can prevent the condition from worsening.
The most effective treatment plans often involve a combination of therapy, medications, and lifestyle changes.
Therapy
Cognitive Behavioral Therapy (CBT) is a common treatment for childhood depression.
It helps children understand and change negative thinking patterns.
Other forms of therapy, such as family therapy or play therapy, may also be effective, depending on the child’s age and circumstances.
Medications
Sometimes, antidepressant medications may be needed, such as selective serotonin reuptake inhibitors (SSRIs).
These medications can help balance brain chemicals that affect mood.
It’s crucial to consult a pediatric psychiatrist to evaluate the child thoroughly and determine the best medication if needed.
Lifestyle changes
Making some lifestyle changes can also support a child’s recovery from depression.
Encouraging regular exercise, a balanced diet, and good sleep habits are important.
These healthy habits can improve a child’s mood and overall well-being.
When to Consult a Mental Health Professional
If a child shows signs of depression, like feeling persistently sad, withdrawing from activities, or losing interest in things they used to enjoy for two weeks or more, it’s important to reach out to a mental health professional.
Early intervention can help prevent long-term emotional challenges and provide the support a child needs to recover and feel better.

Final Thoughts
Childhood depression is a serious issue that needs careful attention.
It can be tough for parents to see their child going through this, but spotting the signs early and getting the right help can truly make a difference.
With the right support, children with depression can overcome their challenges and go on to lead happy, healthy lives.



